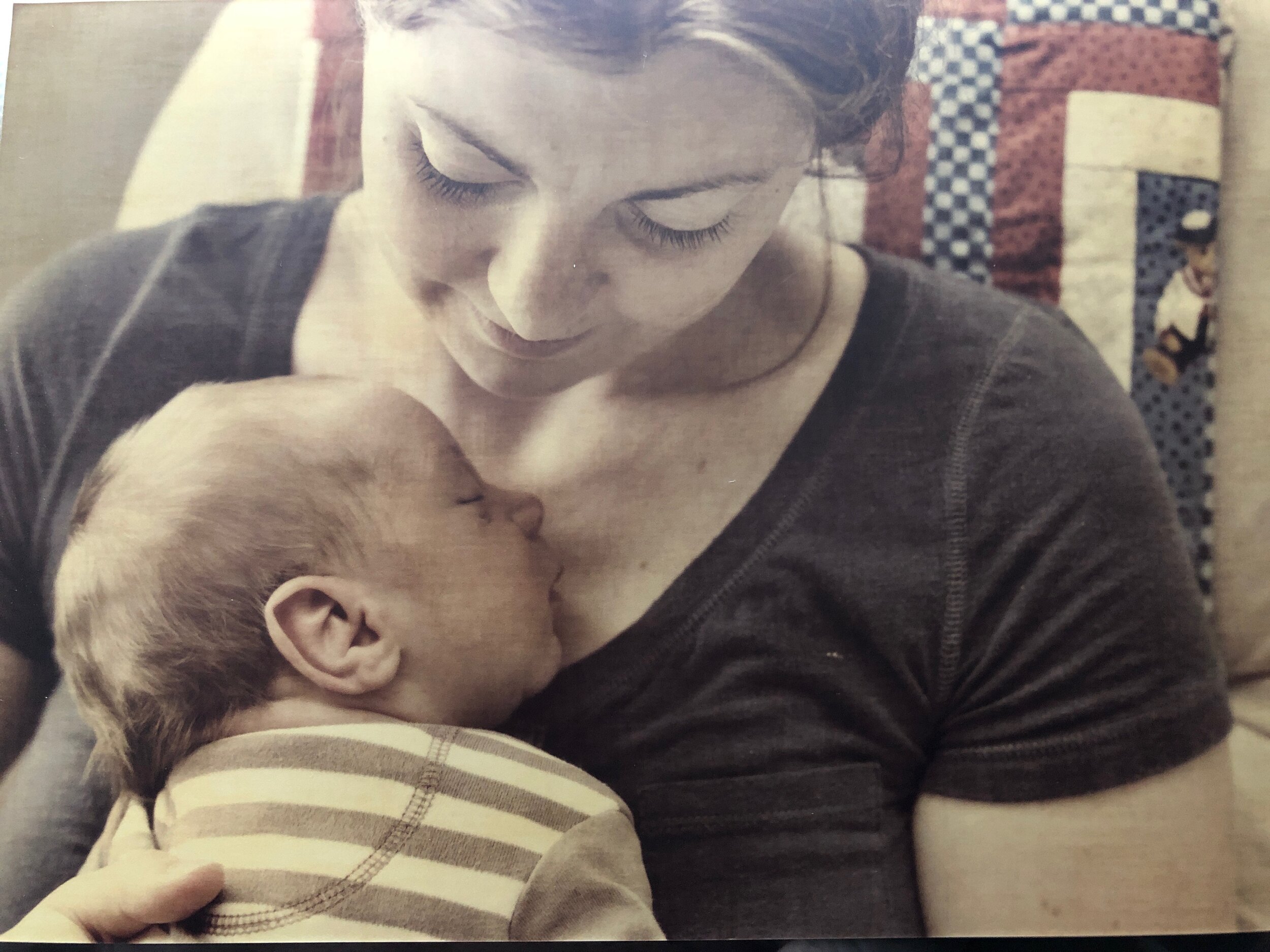
How can an oral restriction affect breastfeeding?
Many oral restrictions are discovered and diagnosed due to difficulties with breastfeeding. An oral restriction can impair a baby’s ability to properly latch, suck, and swallow. If you are having issues such as mastitis, decreasing milk supply, or clogged ducts, or if your baby is having difficulty latching or losing weight, it is a great idea to check if your infant has an oral restriction.
What signs should I look for?
An oral restriction can hamper your baby’s ability to breastfeed, leading to important symptoms for both you and your baby.
You may notice that your baby is:
acting irritable or fussy during or after feeding
experiencing gassiness or frequently spitting up
having difficulty creating a secure latch during nursing
losing weight or having poor weight gain
falling off the breast frequently during nursing
frequent feedings without feeling “satisfied”
If you are nursing your baby, you may notice:
breast pain
plugged milk ducts (which can lead to mastitis)
engorgement
cracked or blistered nipples
a feeling that your baby is chewing or biting on the breast
recurrent thrush or infections
Of course, not all breastfeeding issues are related to an oral restriction. Your lactation consultant can help you find solutions to issues such as milk supply, positioning, shallow latch, inverted or flat nipples etc.
What does tongue tie look like in a baby?
When it comes to oral restrictions, there’s no “one size fits all” presentation. Oral restrictions are diverse in their appearance, which is why it is important to seek care from a healthcare professional who is knowledgeable about this condition.
How common is tongue tie?
It’s hard to say for sure because more research and better statistics are needed. Some research indicates that up to 10 percent of babies are born with an oral restriction and up to 25 percent of nursing infants can be affected by shallow latch caused by this condition. Many oral restrictions go undiagnosed even into adulthood, mainly because of the lack of education among healthcare professionals about this condition.
What is the treatment for an oral restriction?
Oral restrictions can be treated with a quick outpatient procedure to release the tie, sometimes referred to as a tongue tie surgery.
A release procedure known as frenectomy is usually done with a laser and may completely eliminate (“ablate”) the tissue restricting the tongue or lip. This differs from a frenotomy, which is usually done with sterile scissors and involves “clipping” or “snipping” the tissue.
What types of healthcare professionals can help my tongue tied baby?
Lactation consultants are often the first to notice breastfeeding-related symptoms that could point to an oral restriction. Although they cannot diagnose, your lactation consultant can help you by referring you to a Proceduralist who can identify and treat the condition.
Proceduralists are trained and licensed to diagnose oral restrictions and perform the release procedure. They include dentists, doctors, naturopaths, nurse practitioners, and oral surgeons.
When is the best time to diagnose and treat an oral restriction?
As soon as possible! In the best of circumstances, a tongue tied baby can be diagnosed and treated shortly after birth. The longer we wait, the more problems can arise. For example, if a baby’s oral muscles are restricted and they compensate by using other muscles not intended for suck and swallow, the brain quickly memorizes these dysfunctional patterns. Thankfully, with the right support from healthcare professionals, after a release procedure babies can learn healthy suck and swallow patterns. Lactation consultants can provide critical support after a release procedure by helping you adjust your feeding plan and breastfeeding technique.
What causes oral restrictions?
As a fetus develops in the womb, tissue forms to anchor the tongue to the base of the mouth. Usually, this tissue dissolves naturally over time. At around the 12th week of pregnancy all that is left is a small, flexible tether. For reasons that have yet to be fully understood, in some fetuses, this tissue does not dissolve. These babies are born with an oral tether that is especially short, tight or thick.
Although much research is needed to better understand what causes oral restrictions, some evidence points to a genetic mutation known as MTHFR (methylenetetrahydrofolate reductase).
Oral restrictions:
are conditions present at birth
appear to be hereditary
are common in babies who are born prematurely
are common in babies who are born with other mid-line traits like “stork bite” birthmarks
What are the possible long-term effects of tongue tie?
Even small components (such as the tiny tether under your tongue) can affect the entire body over time. Oral restrictions can be indirectly related to a cascade of developmental issues in the mouth and even in the rest of the body.
If left untreated, oral restrictions may affect your child’s:
Much research needed to understand the long term effects of oral restrictions. Some specialists suspect that oral restrictions could play a role in serious, chronic conditions in adulthood such as sleep apnea, asthma and heart problems.
Trust your instincts
It is very common for parents to be dismissed, have their concerns be minimized, or told their baby is not tongue tied because their practitioner lacked specific training and experience in diagnosing oral restrictions.
At the health:latch circle we are advocates for parents and patients. We believe you know your body and your baby better than anyone. Listen to your gut and continue to ask questions until you are satisfied with the answers.
Next steps
As soon as you suspect that tongue tie is a possibility, or even better, if you just want a preventative evaluation - it's time to gather together resources and prepare for the decisions that you will have to make.
You need caring, kind, and knowledgeable professionals who can guide and advise you through the sometimes bumpy road of education, examination, diagnosis, treatment, and follow-up therapy.
Creating your circle of support
We created the health:latch circle as a place for parents like you to surround yourself with support and for providers to connect with parents.
The health:latch circle is a radically kind, community-based online platform that allows interested parents and professionals to learn together and connect to trusted professionals who are committed to helping families thrive.
Learn more about the health:latch circle and create your free parent account here.